What Are Common Herniated Disc Symptoms?
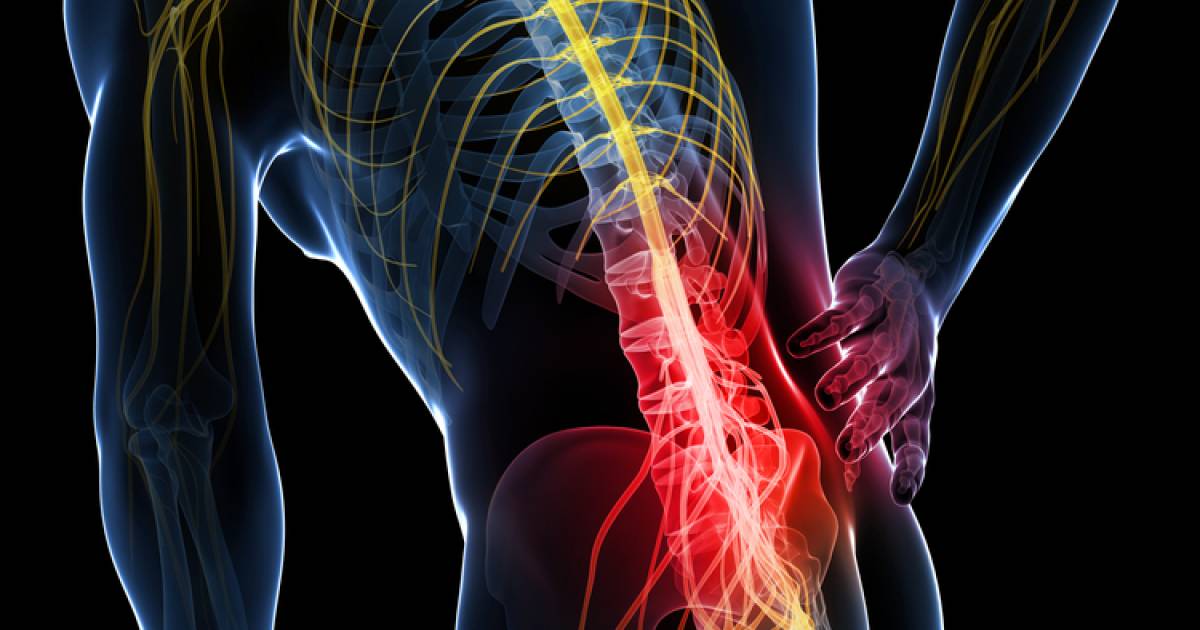
Discs are the shock absorbing elements of the spine, and are found between each vertebra in three areas of the spine: the neck (cervical region), midback (thoracic area), and lower back (lumbar spine). These three regions give our spine mobility. Spinal discs are a cartilaginous ring surrounding an inner jelly. A herniated disc refers to an injury that causes the jelly to squeeze out of place. Disc herniations are most common in individuals from thirty to fifty years old. Youth helps preserve disc function early in life, while age tends to degenerate the discs enough that herniation is unlikely. Get to know the common symptoms of a herniated disc now.
Numbness Or Tingling
Herniated discs come with a myriad of symptoms. Some herniations are completely painless while others cause severe dysfunction. Numbness or tingling (neuralgias) is a common symptom of spinal disc herniations, They can occur together or separate. When the herniated disc is seen in the cervical area, these neuralgias tend to occur in the arms, hands, and fingers. The sensation is often described as a 'falling asleep' or 'pins and needles' sensation. Herniated discs in the lumbar spine impact the legs. Neuralgias occur because there is pressure on the area of the nerve that carries sensation. It is very individualized. A herniated disc in the same area could create numbness in the toe of one individual while causing tingling and pain in the thigh of another.
Learn more about the common signs of a herniated disc now.
Muscle Weakness

When a spinal disc herniates, the jelly that squeezes out can apply pressure to a nerve. Spinal nerves carry pain and other sensations as well as motor function. Direct pressure on the aspect of the nerve that carries motor ability will cause muscle weakness. Herniated discs tend to create weakness in the extremities, and at times the muscle weakness is profound enough to cause visible muscle atrophy. It is not uncommon, however, for a patient to be completely unaware of the muscle weakness. During an examination, a physician is able to isolate individual muscle actions to detect the problem early. It is also possible to have muscle weakness without any other symptom such as pain, numbness, or tingling. Weakness from a herniated disc may be a very serious complication and should always be evaluated by a healthcare professional.
Continue reading to reveal the next symptom of a herniated disc now.